
Diagnostic laboratory in Bangalore supports treatment progress in thalassemia
The new BMT unit built in memory of Mechtild Harf at the Bhagwan Mahaveer Jain Hospital in Bangalore was launched in September. At full capacity, 120 children a year between the ages of 2 and 18, primarily suffering from thalassemia will be treated in the unit operated by our collaboration partner, the Sankalp India Foundation.
3-4% of the Indian population are genetic carriers of thalassemia. Every year, 10,000 children are born with the major form of the inherited disease, which leads to severe anemia. Due to the high financial burden, only 5-10% of thalassemic children receive optimal treatment. Children with this degree of disease are dependent on frequent blood transfusions, and only hematopoietic stem cell transplantation can ultimately cure them.
The affiliated molecular laboratory provides the necessary diagnostics
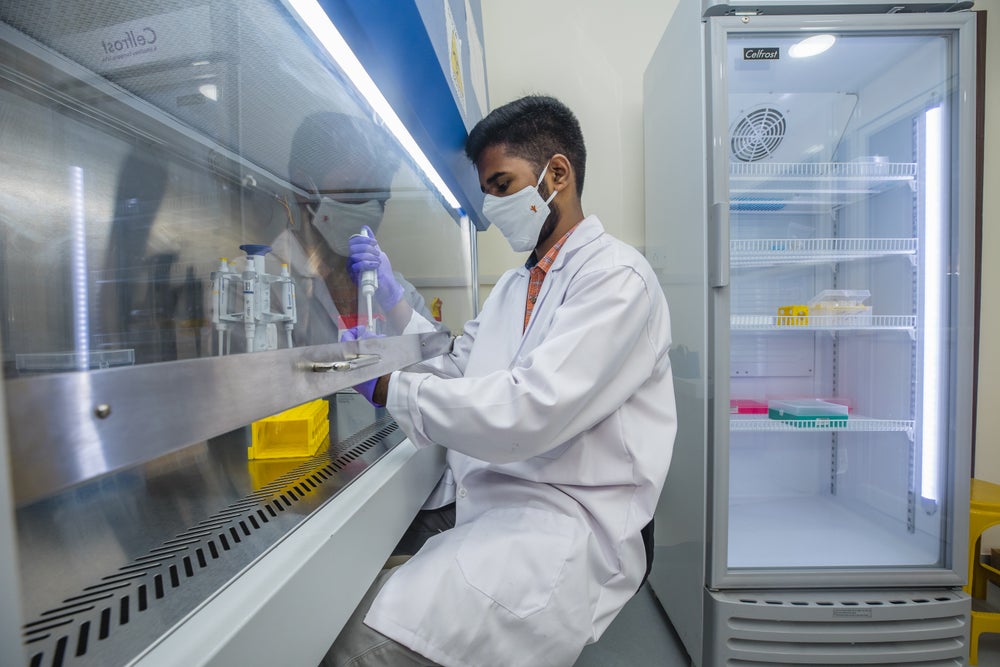
The BMT Center includes a molecular diagnostic laboratory. This laboratory is located next to the pediatric ward and allows for quick and easy in-house testing. It handles all the important genetic analyses needed to determine the children’s disease profiles. These are important for choosing the right treatment as well as for following the engraftment of the transplant after transplantation. In the event that the patient becomes ill during the post-transplantation period, for example due to the spread of microbes or a virus, the laboratory is able to test the patient's samples for a wide range of pathogens using rapid qPCR tests. Only some of the microbiology tests, such as blood cultures to check for antibiotic resistance, are outsourced to highly reliable external partners.
The most important test for thalassemia patients

One of the first and most important tests children receive after admission is a genetic characterization of their disease, which means determining the exact mutations that lead to the defective alleles of β-hemoglobin. Most patients who come to the BMT Center have never had solid testing done. Therefore, it is not even always clear if the patient really has thalassemia. Additionally, this data collection is of great importance in advancing the overall understanding of thalassemia as a genetic disease.
Although up to 30 million people in India have a genetic background of β-thalassemia, the molecular variations have only recently begun to be thoroughly studied. Due to the large number of patients and financial and infrastructural limitations, progress has been slow.
Various mutations can cause thalassemia
There are 10 different mutations known within the β-hemoglobin chain, representing the profile of approximately 90% of patients. The remaining 10% have many different mutations, many of which have never been described.
For the 10 most common mutations – all concerning only a single nucleotide - detection is simple and straightforward. It is done by qPCR using highly reliable primer (oligonucleotides) pairs that are able to distinguish the variable sequence of wild-type and mutant gene alleles. Whenever none of the primer pairs leads to a conclusive result - i.e. no product is amplified - the DNA sequence must be examined with a sequencer to decipher a rare and novel mutation. For this, the lab uses Thermo Fisher's state-of-the-art SeqStudio.
Recognition for thalassemia is increasing
Rajat Kumar Agarwal - responsible for research and quality at Sankalp India Foundation - is pleased with the recent developments regarding the treatment of thalassemia in his country, "Here in India, we are now developing more awareness about the issue. Better diagnostic measures are being offered, and people seem to be properly recognizing and acknowledging the problem."
Further steps are being taken to ensure the best treatment for all
In addition to individual diagnostics, the lab also works in collaboration with scientists who analyze the data statistically. "By examining genetic profiles and related data, such as response to certain drugs, decision-making about who most needs a transplant becomes more efficient," explains Rajat Kumar Agarwal.
"For example, there is a group of patients who responds very well to the drug hydroxyurea. This pharmacological agent increases the production of fetal hemoglobin, the gene of which is completely unaffected by thalassemia. Unfortunately, it is difficult to predict who belongs to this group. This is an area where we hope to improve the situation in the next few years with the help of our data."
He continues, "With this center and diagnostic facility, we are laying the foundation for a better future for all children born with this hereditary disease. One day, every child should be able to be treated properly and the disease should be brought under control.”
“This new diagnostic laboratory is not only wonderful for the patients who will directly benefit from its services, but it also plays a major role in raising the overall standards of care for thalassemia patients through scientific advances,” says Dr. Alexander Schmidt, DKMS Global Chief Medical Officer. “We are ready to support the Sankalp India Foundation in this challenge with the expertise and experience of our Clinical Trials Unit.”